The Hidden Costs of Surgery: How Employers Can Deliver Better Outcomes, Predictable Costs, and Happier Employees

Each year, around 40-50 million surgeries are performed in the U.S. making surgical care one of the most critical and costly areas of the healthcare system (National Library of Medicine, 2020).
In response, employers are seeking comprehensive surgery care experiences that improve surgical outcomes, prioritize provider quality, and enhance healthcare cost efficiency. To realize these goals, benefits leaders need to have the right strategy and support in place. Far too often surgery turns into a financial and logistical challenge for employees, extending beyond the operating room.
Even with employer-sponsored insurance or access to surgical Centers of Excellence, employees still often face roadblocks that keep them from accessing high-quality, affordable surgery care. The hidden costs of surgery are mounting across the industry and impeding improved surgery outcomes for many employers. It’s time to bring these obstacles into the light and transparently discuss how to overcome them.
To validate these observations and dig deeper into the surgery experience, Transcarent surveyed more than 1,000 commercially-insured Americans.* The research revealed concerning post-surgery trends and their impact on outcomes.
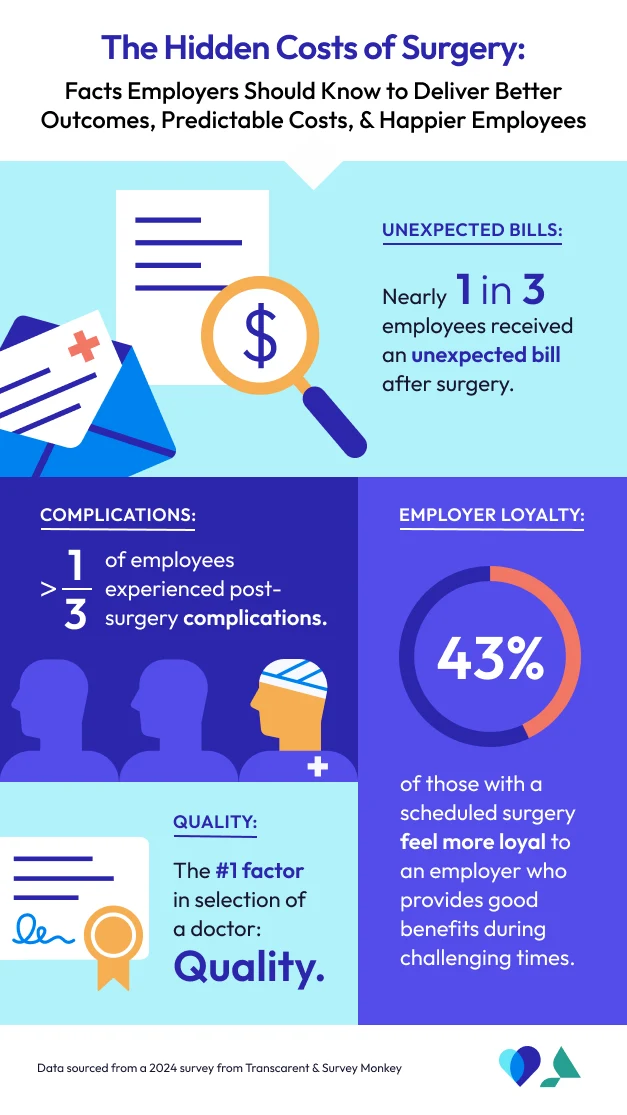
The results highlight several potential factors behind rising healthcare costs for both employees and employers — including unexpected bills, post-surgical complications, and incomplete quality measurements being the biggest culprits.
The survey’s insights reinforce that an emphasis on comprehensive, high-quality care can help align incentives across providers. Rather than rewarding costly, volume-driven services - a value-based approach focused on care delivered by high-quality providers often leads to better outcomes while reducing unnecessary procedures and post-surgical recovery complications.
These findings also highlight the need for employers to reexamine their surgery care benefits. Prioritizing cost predictability and a seamless, comprehensive experience can make the journey easier for employees.
Not only can this result in better surgery outcomes, it can also improve the employee’s overall experience — including increased satisfaction and loyalty. In fact, according to our study, more than half of respondents with a scheduled surgery indicated a strong benefit could influence their decision to switch employers.
Employers have the opportunity to improve employee health outcomes and drive better cost predictability by creating a system where people receive the right surgery care at the right time with the right support.
Here are researched backed tips for how employers can implement this.
1. Predictability Wins: Address Unexpected Bills
Despite growing efforts to improve price transparency in healthcare, the Transcarent study found that nearly one-third of employees who recently had surgery received an unexpected or surprise bill.
What’s the root cause? The standard fee-for-service payment model often results in separate bills from multiple providers — anesthesiologists, surgical assistants, radiologists — some of whom may be out of the employee’s network even when the primary surgeon is covered. This fragmented billing system often leads to confusion and financial stress for employees, and its uncoordinated approach can also result in poor outcomes. Employers need predictability in their costs.
2. Simplify Costs with Predictable Value-Based Bundles
Prospective value-based bundles are designed to make costs more predictable. Combining all the components of a surgical episode—facility, anesthesiologist, surgeon, and other specialists—into one simple, upfront payment, mitigates the risk of out-of-network provider bills slipping through the cracks.
Value-based bundles often include a built-in warranty, ensuring that all providers share the risk if a surgery does not go as planned. This structure incentivizes provider collaboration, aligning their goals to achieve the best possible patient outcomes. And if there is a complication, the providers are responsible for post-operational care, minimizing employer and employee financial burden. By focusing on quality rather than volume, providers work together to reduce additional procedures while maintaining a high standard of care.
3. Reduce the Common Occurrence of Post-Operative Complications
The Transcarent study found more than one-third of employees who had surgery experienced post-operative complications, with 43% seeking emergency room care.
Surgical complications can arise for many reasons - some unavoidable, but others can be preventable, such as failure to follow best practices, improper protocols, or performing unnecessary procedures. When issues occur, many employees turn to the ER - significantly driving up healthcare costs. Interestingly, the Transcarent study uncovered that younger employees reported higher rates of complications than older adults, challenging common assumptions surrounding surgical risks.
Contrary to what you may think, younger patients reporting more post-op complications than older patients is a documented phenomenon in some clinical studies.
But why? It might come down to activity, expectations, and awareness. Younger people tend to get back on their feet faster - sometimes too fast - putting more stress on recovery. They also expect a quicker return to normal, so even small issues stand out. And because they’re more likely to use digital tools to report symptoms, their complications may simply be more visible.
However, no matter the patient’s age, complications can have a compounding effect - resulting in missed workdays, decreased productivity, and increased long-term healthcare expenses.
4. Prioritize Quality at Every Step: Expert Guidance and Rigorous Evaluations for Data-Driven Decisions
Mitigating the risk of complications can be achieved by focusing on three things:
Surgical appropriateness (is the person right for surgery?)
Surgical quality (is the surgeon right for the person?)
Clinical guidance at every stage and in between
To achieve quality care, it’s necessary to solve all three measures. When facing a major health decision, getting a diagnosis and recommendation is the first and most crucial step. However, some providers default to recommending surgery, which is often the costliest option. To counter this, we should empower people receiving care to fully understand all their options by connecting them to expert physicians who deliver unbiased recommendations, whether it’s surgery, physical therapy, or exercise.
Take, for example, an employee dealing with nagging, intermittent knee pain - not urgent, but disruptive enough to affect daily life. Under the status quo, they might be sent down any number of fragmented care paths: an orthopedic surgeon’s office, physical therapy, or even a primary care provider. Each route comes with its own biases, costs, and delays - none providing clear guidance and assurance that any will lead to the right outcome.
Now imagine that same employee has fast, easy virtual access to a top-tier orthopedic physician. Instead of bouncing between providers or defaulting to surgery, they receive an expert, unbiased diagnosis and a clear recommendation for the most effective step - whether that’s surgery, physical therapy, or a home exercise program.
The Result? Confidence, Clarity, and a Faster Route to Recovery
We need to do more to make it easier for those who do require surgery to access high-quality care options. Quality varies across specialties, and evaluations must be nuanced enough to measure the criteria relevant to each patient’s procedure.
Finally, a high-quality surgeon is only one part of the equation. People need comprehensive clinical guidance before and after they leave the operating room. Many complications can be prevented when people are well-prepared and understand the proper pre- and post-operative protocols.
What Employers Can Do
Healthcare spending is predicted to continue rising year-over-year, with inpatient surgeries steadily accounting for 50% of hospital expenditure and 30% of overall healthcare costs (National Library of Medicine, 2021)
The good news is that many of these expenses can be avoided. With early guidance and clinical support, employers can help employees connect with higher-quality providers, reducing unnecessary surgeries and costly complications. Adopting value-based bundles that align incentives also helps drive cost predictability and mitigate surprise bills.
A Comprehensive Solution: Transcarent MSK & Surgery Care
With the largest value-based network and virtual access to care across the entire spectrum - including physical therapy, expert diagnoses, second opinions, and convenient urgent care - Transcarent delivers the One Place for MSK & Surgery Care.
A clinically guided Care Team connects Members to the right care at the right time, and surgery only when necessary. By prioritizing cost transparency and high-quality care, we help eliminate unexpected medical bills and fragmented payment structures.
The entire surgical episode is paid for via one upfront price and care is completely coordinated, reducing the risk of out-of-network charges and post-surgical financial surprises. Employers and employees alike gain peace of mind - knowing they are getting high-quality, cost-effective care without any hidden costs.
Reduce Surgical Costs & Improve Employee Well-Being
Want to drive cost predictability while enhancing employee health? Give your employees access to the right care at the right time with the right support and predictably lower costs through appropriate high-quality surgery care.
Learn more about Transcarent MSK & Surgery Care and see how our comprehensive approach to care and advanced quality methodology surfaces the best clinicians possible for the best outcomes.
*Survey methodology: Survey respondents were targeted and screened for this profile with the following parameters: Lives in the United States, is 18 years or older, currently receives health insurance offered through their employer or a family member’s employer, the employer through which health insurance is offered has over 2000 employees. The survey had 1,115 respondents during the administration period, June 17-26, 2024.
